1. Introduction: The Challenge of Syndromic Presentation
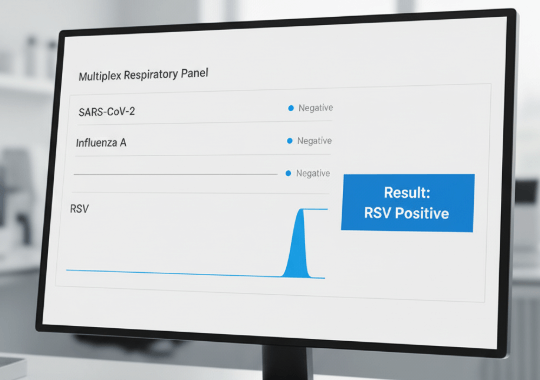
A patient presents in the emergency room with a fever, cough, and sore throat. Is it COVID-19, Influenza A, Influenza B, or RSV? The symptoms are nearly identical, but the implications for treatment, cohorting, and antiviral stewardship are vastly different. This is the classic challenge of a syndromic presentation. The traditional diagnostic pathway, relying on sequential single-analyte tests or a slow central lab panel, is inefficient and ill-suited for a healthcare environment that demands speed and precision [1].
2. The Clinical Imperative for Multiplexing
A single test that provides a comprehensive answer from one sample offers profound clinical advantages. Firstly, it enables rapid, targeted therapy. Knowing the causative agent upfront allows for the immediate initiation of the correct antiviral medication, which is often most effective in the early stages of infection. Secondly, it is a powerful tool for antimicrobial stewardship. A positive viral result can give a clinician the confidence to withhold unnecessary antibiotics, combating the global threat of antimicrobial resistance [2]. Finally, it improves patient outcomes and safety by ensuring correct isolation procedures are implemented immediately, protecting other vulnerable patients and healthcare workers.
3. The Economic Imperative for Multiplexing
The upfront cost of a multiplex test is often higher than a single-analyte test, but its downstream economic benefits are substantial. By reducing the time to diagnosis, multiplex POCT can significantly decrease the length of stay in high-cost settings like the emergency room. This improves patient throughput and frees up capacity. It also reduces overall cost-per-encounter by eliminating the need for multiple, sequential tests and reducing the labor associated with sample recollection and processing. As demonstrated in real-world studies, these workflow efficiencies translate into significant operational savings for healthcare institutions [3].
4. The Technological Hurdle: Why Reliable Multiplexing is Hard
The promise of multiplexing is clear, but the technical execution is fraught with challenges. For a lateral flow assay to detect four distinct targets, it requires four or more perfectly deposited lines of highly specific biological reagents in a very small space. Any microscopic variation in the volume, concentration, or position of these reagents can lead to cross-reactivity (false positives) or a loss of sensitivity (false negatives) for one or more targets. This 'Black Box Risk'—the uncertainty that a test from batch X will perform identically to one from batch Y—has been the primary barrier to clinical trust and widespread adoption.
5. The Solution: Engineering Reliability at the Source
reOpenTest has addressed this fundamental challenge by moving quality control from a post-production check to an integral part of the manufacturing process itself. Our NomoFlow™ platform utilizes AI-driven robotics and real-time optical feedback to deposit reagents with microscopic precision. This process ensures that every line on every test is functionally identical, achieving a batch-to-batch CV of less than 3%. By solving the problem of manufacturing variability, NomoFlow™ provides the verifiable, reliable foundation necessary to deliver the full clinical and economic promise of high-performance multiplex diagnostics.
6. Conclusion
The move toward multiplex point-of-care diagnostics is not a trend, but an essential evolution in response to the demands of modern healthcare. However, for this evolution to succeed, it must be built on a bedrock of trust and reliability. By focusing on manufacturing as the true source of diagnostic certainty, reOpenTest provides the tools clinicians need to make critical decisions with confidence, right where it matters most: at the point of care.